Samenvatting
Jochemsen HM, Caspers PWJ, Gijsen R. Off-label voorschrijven: medisch handelen en motieven van huisartsen. Huisarts Wet 2007;50(5):193-7. Doel In dit onderzoek gingen we na hoe huisartsen omgaan met het off-label voorschrijven van medicijnen, wat hun motieven hiervoor zijn en of zij behoefte hebben aan bepaalde instrumenten bij het voorschrijven. Methode We stuurden 800 huisartsen een vragenlijst. We legden een aantal casus voor en vroegen naar hun eigen handelen. Resultaten Van de 800 huisartsen waren er 13 niet meer praktiserend. Van de resterende 787 huisartsen ontvingen we 464 vragenlijsten terug (respons 59%). Uit de voorgelegde casus bleek dat 100% van de huisartsen off-label voorschrijft. De meest genoemde motieven hiervoor zijn dat de werkzaamheid van het middel is beschreven in huisartsgeneeskundige richtlijnen, in handboeken of in de wetenschappelijke literatuur. Experimenteergedrag komt echter ook voor. Bijna de helft van de huisartsen zegt regelmatig niet te weten of een voorgeschreven middel een geregistreerde toepassing is. Wanneer ze het wel weten, informeert 27% de patiënt daar zelden of nooit over en vraagt de helft zelden of nooit toestemming. De evaluatie door huisartsen is beperkt. Het idee om instrumenten te ontwikkelen die bijdragen aan een welbewuster off-label voorschrijven, kreeg brede steun van de huisartsen. Conclusies De drie meest genoemde motieven om off-label voor te schrijven zijn in lijn met de standpunten van CBG/IGZ en NHG. Het motief dat de off-labeltoepassing is opgenomen in richtlijnen, voldoet tevens aan een eis in de nieuwe Geneesmiddelenwet. Desondanks kunnen sommige aspecten van het huisartsgeneeskundig handelen beter. Ontwikkeling van een aantal instrumenten zou daaraan kunnen bijdragen.
Wat is bekend?
- Artsen schrijven regelmatig medicijnen voor met een andere indicatie dan in de registratietekst van het medicijn staat vermeld (= off-label).
- Off-label voorschrijven kan gewenst zijn, maar kan ook risico op bijwerkingen geven voor de patiënt en overbodige kosten met zich meebrengen.
Wat is nieuw?
- Van de huisartsen zegt 45% lang niet altijd te weten of hun voorschriften wel of niet off-label zijn.
- Een belangrijk motief om off-label voor te schrijven is dat het geneesmiddel geadviseerd wordt in richtlijnen. Soms spelen echter ook riskantere motieven een rol.
- Ruim een kwart van de huisartsen zegt de patiënt zelden of nooit te informeren dat een geneesmiddel off-label is. De helft vraagt zelden of nooit om toestemming aan de patiënt.
- Positieve of negatieve ervaringen met off-label voorschrijven worden nauwelijks systematisch geëvalueerd in de huisartsgeneeskunde. Huisartsen willen wel graag steun bij het voorschrijven en evalueren van off-label medicijngebruik.
Inleiding
Off-label voorschrijven wil zeggen dat een arts een geneesmiddel voorschrijft buiten de geregistreerde toepassing(en).123 Het middel wordt gebruikt voor een andere indicatie, in een andere dosering of voor een andere patiëntencategorie dan de registratietekst van het medicijn vermeldt. Bij dat laatste valt te denken aan kinderen, zwangere vrouwen, personen met bepaalde aandoeningen of personen die bepaalde andere geneesmiddelen gebruiken. Onderzoeken tonen aan dat huisartsen op kleine tot grote schaal geneesmiddelen off-label voorschrijven.456 Soms is off-label voorschrijven gewenst, bijvoorbeeld als er geen alternatieven zijn en de effecten van het middel wetenschappelijk zijn onderbouwd. Dit soort off-labelindicaties zijn meestal opgenomen in de medische en/of farmacotherapeutische richtlijnen. In andere gevallen is het echter niet onderbouwd, en kan het off-label voorschrijven een ongewenst risico op gezondheidsschade voor de patiënt betekenen. Bovendien leidt gebruik van middelen waarvan de werkzaamheid gering of afwezig is tot overbodige kosten in de gezondheidszorg. Het overheidsorgaan College ter Beoordeling van Geneesmiddelen (CBG) heeft samen met de Inspectie voor de Gezondheidszorg (IGZ) een standpunt geformuleerd over goed en slecht off-label voorschrijven.1 Het standpunt van het NHG over verantwoord en af te raden off-labelgebruik sluit hier op aan, en geeft enkele praktische aanbevelingen voor huisartsen.23
Het is onbekend hoe artsen in de praktijk omgaan met off-label voorschrijven. In opdracht van de IGZ heeft het Rijksinstituut voor Volksgezondheid en Milieu (RIVM) een schriftelijke enquête gehouden onder huisartsen en specialisten. Met dit onderzoek wilden we inzicht krijgen in het bewustzijn van artsen bij het off-label voorschrijven, in hun motieven om off-label voor te schrijven, in de mate waarin artsen patiënten informeren en toestemming vragen en hun overwegingen daarbij, en in de manier waarop artsen het off-label voorschrijven evalueren. Daarnaast wilden we inventariseren of er behoefte is aan instrumenten die artsen helpen om bewuster om te gaan met off-label voorschrijven. Het eerste deel van het onderzoek was gericht op huisartsen, het tweede deel (hier niet beschreven) op medisch specialisten.7
Methoden
We ontwikkelden een vragenlijst aan de hand van de hierboven beschreven onderwerpen en op grond van knelpunten bij off-label voorschrijven die in de literatuur zijn beschreven.45678910111213 De vragenlijst begon met een aantal casussen van combinaties van medicijn en indicatie. We vroegen de artsen of zij het medicijn voor de betreffende indicatie in de afgelopen twee jaar hadden voorgeschreven. Hiermee wilden we enerzijds het onderwerp off-label voor de huisartsen concretiseren en anderzijds een indruk krijgen van het vóórkomen van off-label voorschrijven. De vragenlijst is onder huisartsen en medisch specialisten uitgetest, waarna enkele wijzigingen zijn aangebracht.
In oktober 2005 is deze vragenlijst opgestuurd naar een steekproef van 800 aselecte gekozen huisartsen. De vragenlijst was voorzien van een brief van de IGZ en een informatiefolder over off-label voorschrijven. Na drie weken stuurden wij een herinneringsbrief. Om het gevoel gecontroleerd te worden zo klein mogelijk te houden, zijn geen identificerende kenmerken op de vragenlijst opgenomen. Nadeel hiervan was dat wij geen non-response-onderzoek konden uitvoeren.
De gegevens zijn geanalyseerd met behulp van SPSS, versie 12.0.1. De gegevens zijn weergegeven als percentages of als gemiddelde scores en standaarddeviaties (sd) op een 6-punts Likertschaal. De scores hierop hadden de volgende betekenis: 1 = nooit, 2 = zelden, 3 = soms, 4 = regelmatig, 5 = vaak, 6 = altijd.
Resultaten
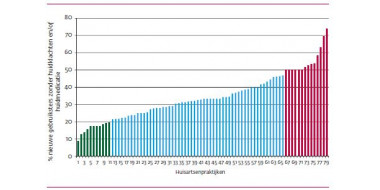
We verstuurden 800 enquêtes naar huisartsen. Daarvan kwamen er 13 oningevuld terug omdat de huisarts niet meer praktiserend bleek te zijn. We ontvingen 464 ingevulde enquêtes (respons 59,0%). Van de deelnemende huisartsen werkte 30% in een solopraktijk, 36% in een duopraktijk, 34% in een groepspraktijk en 9% in een ander type praktijk of als waarnemer in meerdere typen praktijken. Ter vergelijking: van alle Nederlandse huisartsen werkten op 1 januari 2005 respectievelijk 27%, 31% en 42% in een solo-, duo- en groepspraktijk.14 De verdeling van de huisartsen in onze onderzoekspopulatie is dus vergelijkbaar met die in de totale Nederlandse huisartsenpopulatie.
Uit de respons op de voorgelegde casus bleek dat alle huisartsen in één of meer gevallen off-label voorschrijven. Zo zei 94% van de huisartsen orale anticonceptiva voor te schrijven bij dysmenorroe en onregelmatige cyclus. Bètablokkers worden door 95% van de huisartsen voorgeschreven bij examenvrees en tricyclische antidepressiva door 93% van de artsen bij (neuropathische) pijn.
Hoe goed kunnen huisartsen inschatten of hun voorschriften geregistreerde toepassingen betreffen? ‘Vaak of altijd’ zei 55%, 29% zei ‘regelmatig’ en 16% ‘soms’ of ‘zelden’. De gemiddelde score voor de hele groep huisartsen was 4,40 (± 0,92), ofwel tussen regelmatig en vaak in.
Aanbevelingen in richtlijnen, in handboeken en in de wetenschappelijke literatuur waren de meest genoemde motieven om off-label voor te schrijven; 54% van de huisartsen noemde een of meer van deze drie motieven. Eigen ervaringen of die van collega’s bleken ook belangrijk. Motieven die kunnen verwijzen naar experimenteergedrag waren ‘soms’ of ‘zelden’ reden om off-label voor te schrijven. Datzelfde geldt voor gevoelens van onmacht en aandringen door de patiënt. Naast deze aangereikte motieven noemden artsen zelf nog: het middel is in het buitenland wél geregistreerd voor de betreffende toepassing, de diagnose is niet altijd duidelijk afgrensbaar (bijvoorbeeld bij artrose en gewrichtspijn) en het middel blijkt goed te werken in de palliatieve zorg. Een overzicht van de motieven staat in tabel 1 op de website (www.nhg.org/henwextra).
We vroegen de artsen of zij hun patiënten informeren wanneer ze bewust off-label voorschrijven. Hierop antwoordde 10% van de huisartsen dat altijd te doen; 27% doet dat zelden of nooit. De gemiddelde score voor de hele groep huisartsen is 3,53 (± 1,45): tussen soms en regelmatig in. De belangrijkste overweging om wel te informeren is de opvatting dat patiënten gewoon horen te weten of zij een off-labelvoorschrift krijgen. Voor veel huisartsen hangt het af van de omstandigheden of ze de patiënt informeren: de kans op bijwerkingen, het ingeschatte intellect en de mondigheid van de patiënt, en beschikbare tijd. Zie tabel 2 op www.nhg.org/henwextra.
Een andere vraag was of huisartsen hun patiënten of de apotheek informeren over specifieke zaken bij een off-labelvoorschrift. Hoewel 32% zegt de patiënt vaak of altijd te informeren over het feit dat de toepassing niet in de bijsluiter staat, doet 28% dit zelden of nooit. Enkele huisartsen opperden het idee om informatie over off-labelindicaties op te nemen in bijsluiterteksten. De helft van de huisartsen zegt zelden tot nooit toestemming aan de patiënt te vragen, en 80% procent informeert zelden tot nooit de apotheek via vermelding van de indicatie op het recept. Tabel 3 (op www.nhg.org/henwextra) laat zien hoeveel artsen de apotheek informeren en toestemming vragen aan hun patiënt.
Uit tabel 4 blijkt dat huisartsen weinig evalueren. Met name het breder beschikbaar maken van ervaringen (structureel evalueren binnen de beroepsgroep of insturen voor publicatie) gebeurt zelden tot nooit.
De behoefte aan instrumenten die meer inzicht geven in het off-label voorschrijven van geneesmiddelen was groot: 89% van de huisartsen had hier belangstelling voor. Wij stelden enkele instrumenten voor (de percentages representeren de belangstellenden): een off-label bespreking in een fto/geneesmiddelencommissie (74%), een meld- en evaluatiepunt, eventueel leidend tot een database en beoordeling (67%) en een off-labelmelding in het elektronisch voorschrijfsysteem (65%). Daarnaast kwamen er nog enkele voorstellen van individuele huisartsen.
| Manieren van evalueren | Gemiddelde score | Sd | Percentage artsen dat deze manier vaak/altijd toepast |
| Ervaringen met off-labeltoepassingen uitwisselen met collega-artsen | 2,97 | 1,08 | 9,1 |
| Eigen ervaringen structureel evalueren bij elke off-labeltoepassing (effectiviteit/bijwerkingen) | 2,78 | 1,44 | 14,3 |
| Een consult inplannen | 2,67 | 1,40 | 12,6 |
| Ervaringen met off-labeltoepassingen structureel evalueren binnen de beroepsgroep | 2,15 | 1,01 | 3,3 |
| Case-reports insturen voor publicatie in de vakliteratuur | 1,16 | 0,43 | 0,0 |
Beschouwing
Representativiteit
Ongeveer 10% van alle huisartsen was uitgenodigd voor deelname aan het onderzoek; de nettorespons was bijna 60%. Dit is te vergelijken met percentages die wij zagen in andere Nederlandse onderzoeken onder huisartsen (41-86%). De aselecte steekproef vormde qua praktijkvorm een representatieve afspiegeling van de Nederlandse huisartsenpopulatie.
Het is niet bekend in hoeverre er selectieve respons optrad en in welke mate dit de resultaten vertekende. Het is wel voorstelbaar dat hiervan sprake was, bijvoorbeeld omdat huisartsen die terughoudender zijn om hun handelen inzichtelijk te maken, wellicht minder vaak hun patiënten informeren over off-labelvoorschriften.
Dit onderzoek richtte zich expliciet op het bewustzijn, de motieven en het handelen vanuit het perspectief van de huisarts. Ongetwijfeld zullen deels sociaal wenselijke antwoorden zijn gegeven. Met de garantie van absolute anonimiteit en de uitgebreide toelichting in de meegezonden brief en folder, hebben we echter geprobeerd om dit zo veel mogelijk te beperken. Uit de antwoorden op de casus konden we concluderen dat niet alleen sociaal wenselijke antwoorden zijn ingevuld.
Bewustzijn
Van de huisartsen zei 45% dat zij zich lang niet altijd bewust zijn van het off-label voorschrijven. Bewustzijn is echter belangrijk om verantwoord off-label voor te schrijven.2 Wij peilden de behoefte aan instrumenten om het bewustzijn te vergroten. Op de suggestie om een off-labelmelding in te bouwen in de voorschrijfmodule van het Huisarts Informatie Systeem (HIS), eerder voorgesteld door Beijer en Gebhardt,1516 reageerde 65% van de huisartsen positief. Een off-label bespreking in het farmacotherapeutisch overleg werd ondersteund door 74% van de huisartsen. Een goede bespreking van effectieve off-labeltoepassingen in bijvoorbeeld het Farmacotherapeutisch Kompas, geopperd door twee huisartsen, lijkt ook een goede suggestie. Bespreking gebeurt nu ook al, maar is erg onvolledig. Een andere suggestie was om in het onderwijs on- en off-label voorschrijven duidelijker te onderscheiden.
Motieven
De belangrijkste motieven om off-label voor te schrijven, zijn beschrijvingen van de werkzaamheid in richtlijnen, in handboeken en in de wetenschappelijke literatuur. Deze motieven zijn in lijn met de standpunten van CBG/IGZ en NHG. Zij stellen dat off-label voorschrijven verantwoord is als er geen goed alternatief beschikbaar is en als het middel wordt voorgeschreven op basis van wetenschappelijk bewijs.123 Het motief dat de toepassing is beschreven in de richtlijnen van de beroepsgroep voldoet ook aan de eis voor off-labelgebruik in de nieuwe Geneesmiddelenwet, die medio 2007 in werking treedt.17 Uit ons onderzoek bleek dat huisartsen zelden off-label voorschrijven uit nieuwsgierigheid naar de werking van een nieuw geneesmiddel, iets wat als een experimentele behandeling moet worden beschouwd. Sommige motieven verwezen wat indirecter naar experimenteergedrag: ‘Op basis van geregistreerde indicaties zou het kunnen helpen’ en ‘Volgens het werkingsmechanisme zou het kunnen helpen’. Deze speelden wel regelmatig een rol. Opvallend was de hoge score van het motief ‘volgens eigen ervaringen werkzaam’ (‘regelmatig tot vaak’). Een goede of slechte ervaring met een middel bij een eigen patiënt maakt blijkbaar veel indruk.
Informeren en toestemming vragen
Uit dit onderzoek bleek dat huisartsen hun patiënten slechts ‘soms tot regelmatig’ informeren als zij een middel off-label voorschrijven. Bijna eenderde (28%) informeert zelden of nooit. Dit ondanks de informatieplicht en de heersende mening van huisartsen dat patiënten het gewoon horen te weten. Net zo vaak (of net zo weinig) wordt een patiënt gewezen op het feit dat de toepassing niet in de bijsluiter staat beschreven. De huisarts vraagt de patiënt slechts ‘soms’ om toestemming (informed consent).
Volgens de Wet op de geneeskundige behandelingsovereenkomst (WGBO) zijn artsen verplicht om de patiënt informatie te geven over de voorgestelde behandeling en moeten zij de patiënt toestemming vragen voor een behandeling.1718 Dit geldt zeker bij off-label voorschrijven, zoals blijkt uit een uitspraak van het Centraal Medisch Tuchtcollege over een casus waarbij nifedipine als weeënremmer werd voorgeschreven.19 CBG/IGZ en NHG vroegen onlangs ook nog eens aandacht voor het informeren en toestemming vragen.123
Mondelinge informatie onthouden patiënten over het algemeen slecht of verkeerd.20 Daarom verdient het de voorkeur patiënten ook schriftelijk te informeren. Het NHG zou het initiatief kunnen nemen om voor veel voorgeschreven off-labeltoepassingen patiëntenbrieven en -folders te maken, vergelijkbaar met de NHG-patiëntenbrieven en -folders voor gezondheidsproblemen. Dergelijke informatie kan op dit moment niet in bijsluiters opgenomen worden, omdat die alleen informatie over geregistreerde indicaties mogen bevatten.
Het overgrote merendeel van de huisartsen zei ‘zelden of nooit’ de apotheker te informeren over het off-label voorschrijven door de indicatie op het recept te vermelden. Onlangs werd ook al vastgesteld dat huisartsen negatief staan tegenover het algemeen informeren van de apotheker over relevante indicaties bij de patiënt.21 Dit heeft ongetwijfeld te maken met de professionele autonomie van de arts en de vertrouwensrelatie tussen arts en patiënt die op deze manier geschaad zou worden.16 Het gevolg is dat de apotheker bij off-label voorschrijven zijn taken medicatiebewaking, doseringscontrole en voorlichting niet optimaal kan uitvoeren. Om uit deze patstelling te komen, is geopperd om een attitudeverandering bij artsen te stimuleren. Zij zouden in een vroeger stadium met de apotheker kunnen overleggen, bijvoorbeeld telefonisch,22 of alleen bij off-labelvoorschriften de indicatie op het recept kunnen vermelden.12 Inmiddels heeft de overheid de gangbare praktijk aangepakt met de volgende expliciete passage in de nieuwe Geneesmiddelenwet: ‘Het buiten de door het College geregistreerde indicaties voorschrijven van geneesmiddelen is alleen geoorloofd wanneer daarover binnen de beroepsgroep protocollen of standaarden zijn ontwikkeld. Als de protocollen en standaarden nog in ontwikkeling zijn, is overleg tussen de behandelend arts en apotheker noodzakelijk.’ Deze regelgeving sluit aan bij die van de nieuwe WGBO. Met invoering daarvan (ook medio 2007) zal de openbaar apotheker als behandelaar verplicht worden verantwoorde zorg te leveren en de patiënt goed te informeren over de behandeling.1723
Evalueren
Het zelf of met directe collega’s evalueren van off-labeltoepassingen gebeurt slechts ‘zelden tot soms’. Wel gaven veel huisartsen aan dat ze geen extra consult inplannen, maar dat ze normaal gesproken iedere patiënt vragen om terug te komen bij aanhoudende klachten of (ernstige) bijwerkingen. Dit vraagt echter wel mondigheid en assertiviteit van de patiënt. Niet alle patiënten komen snel terug wanneer het geneesmiddel niet schijnt te helpen of wanneer ze last krijgen van bijwerkingen. Structureel evalueren binnen de beroepsgroep gebeurt zelden. Er bestaat bijvoorbeeld geen register waarin artsen ervaringen kunnen melden en waardoor ze informatie die nu verdeeld is over individuele artsen, systematisch kunnen evalueren. Aan zo’n register bleek wel behoefte te zijn.
Conclusie
In dit onderzoek gaf een aanzienlijk aantal Nederlandse huisartsen inzicht in hun voorschrijfgedrag. Het belangrijkste motief om off-label voor te schrijven – de werkzaamheid is wetenschappelijk onderbouwd – is in lijn met het standpunt van de overheid en het NHG. Het motief dat de off-labeltoepassing is opgenomen in richtlijnen, voldoet aan de eis die de nieuwe Geneesmiddelenwet aan off-labelgebruik stelt. Op een aantal aspecten zou het off-label voorschrijven echter beter kunnen. De ontwikkeling van enkele instrumenten kan het voor huisartsen gemakkelijker maken om bewuster voor te schrijven en als groep meer kennis op te bouwen over de waarde van off-label voorgeschreven geneesmiddelen. Hiervoor is wel inspanning vereist van verschillende organisaties, zoals NHG, KNMP, DGV, CVZ en medische faculteiten.
Literatuur
- 1.↲↲↲↲College ter Beoordeling van Geneesmiddelen en Inspectie voor de Gezondheidszorg. Verantwoord off-label voorschrijven mag. www.cbg-meb.nl/nl/nieuws, 18 februari 2005.
- 2.↲↲↲↲↲NHG. Aanbevelingen voor het off label voorschrijven van geneesmiddelen. NHG-Standpunt. Utrecht, juni 2005. www.nhg.org.
- 3.↲↲↲↲Folmer H. Plaats van ‘off-label’ voorschrijven van geneesmiddelen. Huisarts Wet 2005;48:235.
- 4.↲↲Radley DC, Finkelstein SN, Stafford RS. Off-label prescribing among office-based physicians. Arch Intern Med 2006;166:1021-6.
- 5.↲↲Van Dijk L, Florentinus S, De Jong A, Velthove K, Heerdink R, Kallewaard M. Het voorschrijven van nieuwe geneesmiddelen in de huisartspraktijk: voorschrijfvolume en off-label voorschrijven. Utrecht: NIVEL, 2003.
- 6.↲↲Schirm E, Tobi H, De Jong-van den Berg LTW. Risk factors for unlicensed and off-label drug use in children outside the hospital. Pediatrics 2003;111:291-5.
- 7.↲↲Caspers PWJ, Gijsen R. Off-label. Transparantie gewenst. RIVM rapport 370050001/2007. Bilthoven: RIVM, in voorbereiding.
- 8.↲Van Dijk L, De Jong A, Florentinus S, Verheij R. Off-label voorschrijven in de huisartspraktijk. Therapeutisch probleem of academisch probleem? Pharm Weekbl 2004;139:902-5.
- 9.↲Haaijer-Ruskamp FM, Denig P. Invloeden bij het kiezen van geneesmiddelen. Gebu 2001;35:37-43.
- 10.↲Hekster YA, Lisman JA, Heijmenberg GM, Koopmans PP, Loenhout JWA. Het voorschrijven en afleveren van geneesmiddelen buiten de geregistreerde indicatie. Gebu 2000;34:139-47.
- 11.↲Koomen JM. Hoe kan de geneesmiddelkeuze worden geoptimaliseerd? Knelpunten en oplossingen. Med Contact 1998;53:1302-5.
- 12.↲↲Lisman J. Voorbij goed en kwaad. Off-label mag, maar niet zomaar. Pharm Weekbl 2004;139:895-9.
- 13.↲De Metz JE, Stroo M. Signalement. Off-label gebruik van geneesmiddelen. Utrecht: DGV, Nederlands instituut voor verantwoord medicijngebruik, 2002.
- 14.↲Kenens RJ, Hingstman L. Cijfers uit de registratie van huisartsen en huisartsen in opleiding - peiling 2005. Utrecht: NIVEL, 2005. www.nivel.nl/pdf/cijfers-uit-de-registratie-van-huisartsen-peiling-2005.pdf.
- 15.↲Beijer HJM. Off-label-gebruik, gewenst of ongewenst? Multidimensionele verwarring niet snel op te lossen. Pharm Weekbl 2003;138:1716-21.
- 16.↲↲Gebhardt DOE. Off-label voorschrijven schept verplichtingen. Arts moet risico’s uitvoeriger met patiënt bespreken. Med Contact 2004;59:377-8.
- 17.↲↲↲Eerste Kamer. Verslag van de vergadering over - het wetsvoorstel Vaststelling van een nieuwe Geneesmiddelenwet (29359); en - het wetsvoorstel Wijziging van Hoofdstuk III van de Wet op de Geneesmiddelenvoorziening en van afdeling 5 van titel 7 van Boek 7 van het Burgerlijk Wetboek (28494). Vergaderjaar 2006-2007. (Voorgaande stukken in te zien op http://parlando.sdu.nl, na invoeren van de nummers 29395 of 28494).
- 18.↲Burgerlijk Wetboek. Boek 7 Bijzondere overeenkomsten, Titel 7 Opdracht, Afdeling 5, De overeenkomst inzake geneeskundige behandeling; Wet geneeskundige behandelingsovereenkomst. Wet van 17 november 1994. Staatsblad 1994, 837.
- 19.↲Uitspraak Centraal Medisch Tuchtcollege. Staatscourant 1998(67):14. Ook gepubliceerd in: Med Contact 1999;54:108-11.
- 20.↲Pieterse BMM, Blom AThG. Een onderzoek naar de wijze waarop patiënten geneesmiddelinformatie interpreteren. Pharm Weekbl 1983;118:789-95.
- 21.↲Muijrers PE, Knottnerus JA, Sijbrandij J, Janknegt R, Grol RP. Changing relationships: attitudes and opinions of general practitioners and pharmacists regarding the role of the community pharmacist. Pharm World Sci 2003;25:235-41.
- 22.↲Tent M, redactie. CBG wil van een oplossing geen probleem maken. “Wie off-label voorschrijft moet goed weten waarom de indicatie beperkt is”. Pharm Weekbl 2004;139:900-1.
- 23.↲Rendering J. Rechten patiënt in de apotheek flink verstevigd. WGBO maakt van apotheker géén medebehandelaar. Pharm Weekbl 2006;141:931-4.
Reacties
Er zijn nog geen reacties.